
The choice of the external fixator is based on:
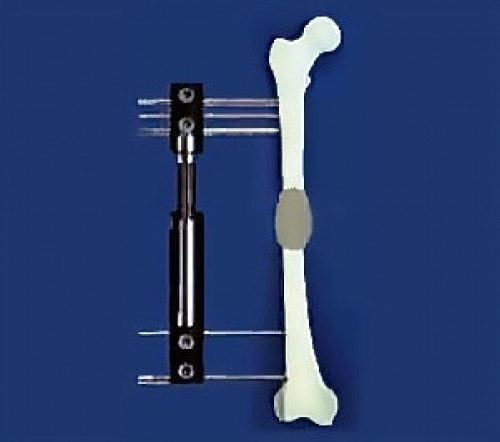
The external fixator is an apparatus external to the organism fixed to the bones by means of pins or screws, through the soft tissues. There are different types of external fasteners : UNILATERAL FIXERS CIRCULAR FIXATORS
They are placed on one side of the limb. At thigh level, they are placed on the outside. At leg level, they are placed inside it.
There are many products: Orthofix fixator, Heidelberg, Judet, Wagner, FSA, etc. The external parts (fixator body), connected to the bone by means of screws or large-caliber pins (4-6 mm), are well tolerated by patients.
They allow a better stability of bone fragments compared to unilateral fixators, with the use of small pins in tension (1.5 -2 mm), but are less comfortable. They allow more complex corrections, obtained gradually in the postoperative phase.
The first fixator was designed by Ilizarov who encoded the method of stretching the limbs. Ilizarov used the principle of the bicycle in which the wheel is held in the center thanks to tension pins, and thus lightening the system you get a great stability, if you respect the basic principles.
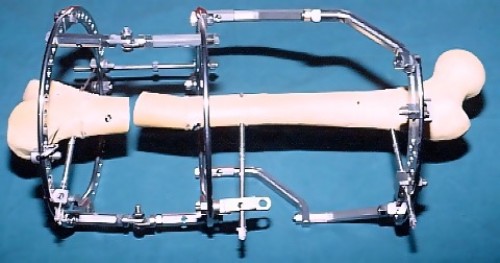
External fixators, in theory, can gradually correct all planes (and deformations). However, the complexity of some deformations, with multiple angles and in different parts within the same bone, sometimes render the theory unenforceable. For example, at foot level which is formed by three parts (forefoot, midfoot and hindfoot), each with numerous bones, deformations must be corrected separately for each part, which in turn must be corrected in the three planes of space separately. At a later stage, their relationship in at least one spatial plane must also be corrected, resulting in an overall correction of 3 x 3 + 2 = 11 spatial planes. Clearly it is difficult to find an external fixator equipped with 11 "hinges" (or rotation centers), which allow to correct deformations in all spatial planes. In addition, you select the most important plans to correct. For long bones, varism/valgism, flexum/recurvatum, translation, rotation, and bone elongation can be corrected simultaneously or sequentially. Such corrections may occur progressively, but sometimes one or two plans are preferred to be implemented simultaneously during the intervention and the progressive correction is reserved for one or two additional plans.
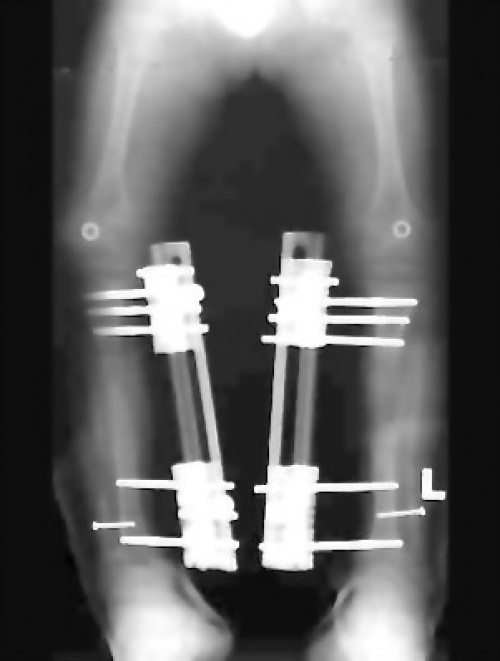
LENGTHENING The distraction depends on the increase. Usually you calculate 1 mm increase/day. For 6 cm, you calculate 2 months. During this phase, you can theoretically walk on your external fixator, except in special cases. However, the external fixator is often uncomfortable and the patient does not normally walk (run errands, etc.). Bone demineralization shows lack of bone stimulation of gait. PROGRESSIVE (ISOLATED) BONE AXIS CORRECTION The Gradual correction generally lasts less than one month. In the case of a complete pre-operative correction fixed by an external fixator, no subsequent progressive correction is required.
Generally, the elongation takes place in different phases :
The fixation lasts about 1 month/cm of increase. Thus, for 6 cm, 6 months of fixation are calculated. The muscles relax and adapt to their new length. Often the patient begins to walk better. The bone strengthens sufficiently to allow ablation of the external fixator.
Dynamization is the phase in which all the nuts are loosened so that the forces, during muscular activity and walking, no longer pass through the external fixator but through the bone. By doing so, the bone receives all the mechanical forces and can strengthen its structure more easily. For many teams, this phase takes about one month, but in case of distraction at 60-300 times/day, this phase is eliminated.
The duration of the use of chalk or orthosis is about one month, but sometimes this phase can be avoided.
The recovery of the activities is progressive with resumption of the gait. Sport is generally not recommended the month following the ablation of the fixer, for risk of fracture of the regenerated bone. The total duration for an elongation of 8-10 cm is 10-18 months with a fixer.
It foresees the following phases :
The Fixation usually lasts about 3 months in the absence of bone elongation, which corresponds to the delay of the consolidation of a fracture.
The Dynamization often precedes the ablation of the external fixator.
By definition, external fixators have pins/screws that pass through soft tissues and put in contact the external environment, considered dirty, contaminated, with the clean, sterile internal environment. Wearing an external fixator for a long time implies an infectious risk that generally occurs around the pins. For this reason, special care and regular visits of the surgeon are needed during lengthening or correction. Initially the visits are weekly or every two weeks, then they are more spaced in time. The patient should protect himself from the risks of dirt and clean himself, or bathe in a certain way (the metal used does not rust). Every day you will have to turn the nuts to make the correction or stretching. Typically, the increase is 1 mm correction per day obtained in four times in the day. Lengthening operations are generally few or not painful. Acting outside of his body (dice), the patient will have few psychological fears and stress. However, stretching the soft tissues on the pins/screws of the external fixator can cause moderate to very moderate pain. The care of the pins must be performed very well to eliminate the risk of complications on them.
Complications can be divided into groups. They are often more serious in elongations, especially those that exceed 15% of the initial length of the elongated bone, and derive from the inevitable ambivalence of external fixators: they must be worn as long as possible, so that the bone becomes very solid, but at the same time, they must be brought as soon as possible, to avoid the risk of infection. INFECTIONS JOINT RIGIDITY DEVIATIONS OF AXIS FRACTURES OSTEOPENIA/OSTEOPOROSIS NERVE OR VASCULAR INJURY POSTOPERATIVE
These are the most frequent complications. Usually located around the pins, with small secretions, they react well to local treatments and antibiotics. They rarely require a new surgery for a pin problem.
Due to the presence of the pins, the soft tissues cannot move easily, so you can find stiffness or decrease in joint mobility. In general, the rigidity slowly regresses after the ablation of the external fixator, but sometimes, 1 or 2 years are needed to recover a normal joint mobility.
Controlling the axis of the bones, although you can act easily on the external fixator, is not easy. After the removal of the fixator, the bone is still in full construction and remodeling, therefore more plastic and deformable. Secondary deviations by bending are sometimes found on the brittle bone. Fortunately, these serious problems rarely require a new intervention, however, it is often necessary a period of fixation in a plaster, after the ablation of the external fixator, for the bone to become more mechanically solid.
They are rare (about 10% or less than 10%), but justify a temporary fixation in the gypsum after ablation of the external fixator.
It is inevitable and manifests itself with a decalcification visible on the X-ray: the bone becomes transparent. After the ablation of the outer fixator, the bone resumes a higher quality density.
The Russians of the Ilizarov Institute have obtained the total amount of calcium of the organism in the elongations by means of external fixators. The loss of calcium is 10% of the total body content (100 gr). This justifies calcium and vitamin supplementation (Vit. D) throughout the lengthening.
Lesions may be directed (rare, during surgery) or secondary by stretching of soft tissues. In general, when this happens, the elongation is interrupted or the elongated bone is retracted, and the recovery takes place progressively.
Wearing an external fixator can be tiring at least at the beginning and for some patients, it represents a "shock" not so much physical as psychological: the child often hides the limb with the external fixator, but soon, he will learn to get used to it. The treatment is long and the patient will go through different psychological stages. Sometimes, in the child you may also experience a masked depressive phase. A fortiori, strong family support is needed, without giving rise to overprotective infantilisms, and sometimes even the help of a psychologist. All long treatments (such as leukemia or tumors) leave signs in the child that can have consequences on his psychological experience and affect him in adulthood. The relational aspect in adulthood can be influenced by the treatments that the child has undergone.
Weymouth Street Hospital
42-46 Weymouth St.
London W1G 6DR, UK
Phoenix Hospital Group
9 Harley Street
London W1G 9QY, UK
Harley Street Specialist Hospital
18-22 Queen Anne St.
London W1G 8HU, UK
Studio Dr. Guichet
Corso Magenta, 44
20123 Milano, IT
+39 0236758514